Why Payer Behavior Is Quietly Changing in Behavioral Health
And Why Most Programs Won’t Notice Until Cash Flow Suffers
Executive Summary
Behavioral health reimbursement is changing — without announcements, policy updates, or clear signals from payers.
Most treatment programs believe they are compliant, properly authorized, and billing correctly. Yet many are experiencing:
- Slower payments
- Increasing underpayments
- Higher documentation scrutiny
- More aggressive utilization management
This is not accidental. It is strategic payer behavior.
The programs that adapt early preserve margins and leverage. The ones that don’t are forced into reactive appeals, staffing cuts, or unfavorable contract renegotiations.
The Myth: “If We’re Doing Everything Right, We’ll Get Paid”
For years, behavioral health providers were taught that reimbursement outcomes were largely a function of:
- Clean claims
- Proper authorizations
- Medical necessity documentation
Those factors still matter — but they are no longer sufficient.
Payers have shifted from overt denial strategies to subtle financial pressure mechanisms that are harder to detect and easier to justify.
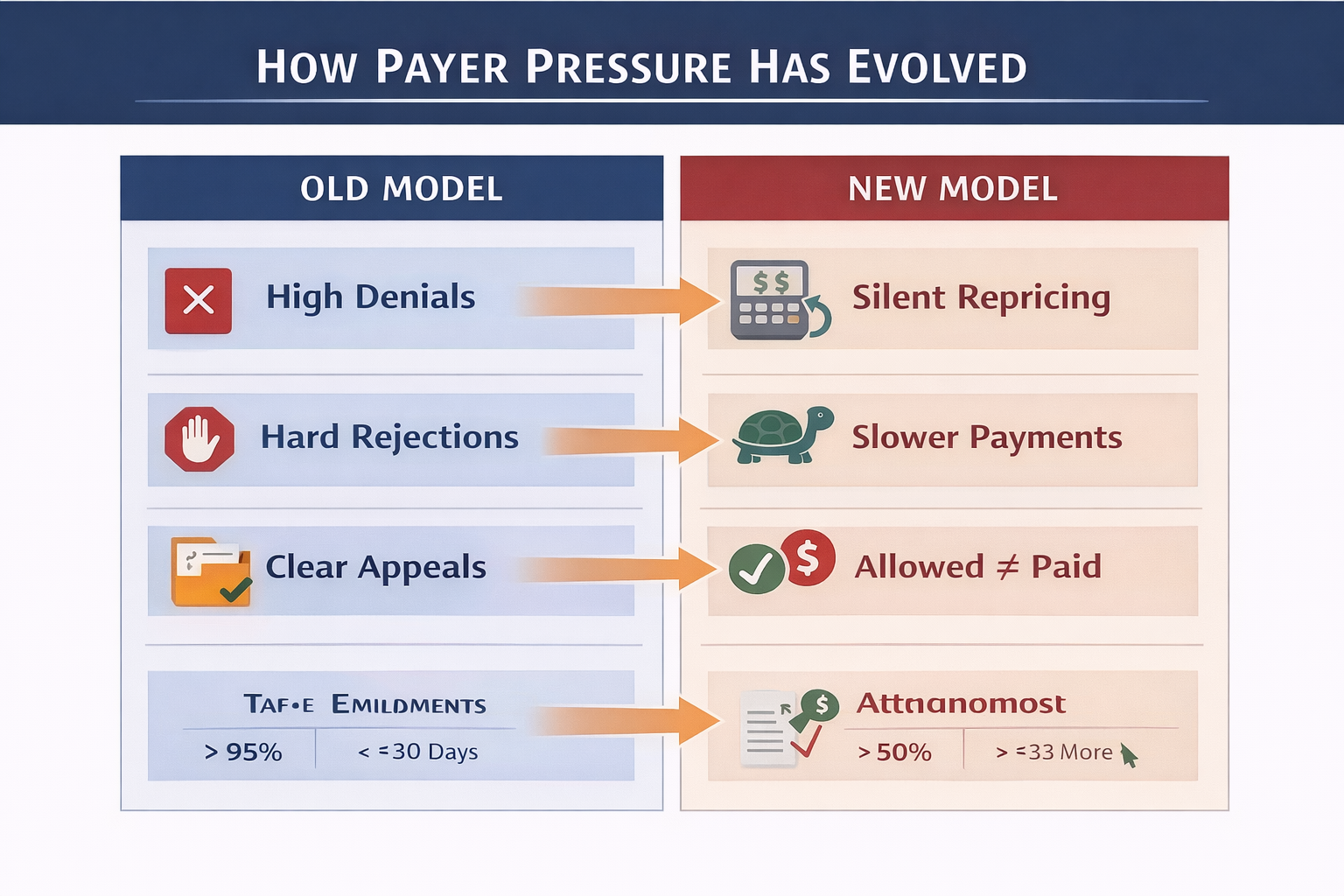
How Payer Behavior Is Actually Changing
1. Denials Are Decreasing — But Revenue Is Still Leaking
Many programs report stable or even improved denial rates while overall collections quietly decline.
Why?
- Claims are approved but repriced downward
- Per-diem rates are silently reduced
- Allowed amounts no longer match historical norms
This creates a false sense of security.
Low denials do not mean healthy reimbursement.
2. Repricing Vendors Are Expanding Their Reach
Third-party repricing entities are now deeply embedded in payer workflows, particularly for:
- Out-of-network claims
- Behavioral health residential and PHP levels of care
- High-cost or long-stay episodes
The result:
- Payments based on payer-defined “reasonable” benchmarks
- Significant gaps between billed, allowed, and paid amounts
- Increased burden on providers to justify market value
Programs that do not actively negotiate repriced claims are accepting rate reductions by default.
3. Utilization Management Is Becoming Financially Motivated
Authorization decisions are increasingly influenced by:
- Internal payer cost targets
- Episode cost modeling
- Historical provider utilization patterns
This shows up as:
- Shorter initial authorizations
- More frequent concurrent review pressure
- Increased demand for progress justification
Programs that lack outcome data and utilization discipline lose ground quickly.
4. Payment Speed Is Now a Leverage Tool
Rather than denying claims, many payers now apply pressure through payment velocity:
- Slower adjudication
- Extended payment cycles
- Increased documentation “clarification” requests
The impact is real:
- Cash flow volatility
- Heavier AR balances
- Greater reliance on credit or reserves
Payment speed is no longer operational noise — it is a strategic variable.
What High-Performing Programs Are Doing Differently
They Track Payer Behavior — Not Just Internal Performance
Sophisticated programs monitor:
- Days to payment by payer and level of care
- Allowed vs paid variance trends
- Repricing frequency by payer
- Appeal success rates by payer
This allows leadership to answer:
“Which payer is quietly becoming more expensive to work with?”
They Treat Underpayments as Strategic Risk
Underpayments are now often larger than denials in total revenue impact.
High-performing organizations:
- Audit underpayments monthly
- Escalate repricing negotiations early
- Use historical rate data to anchor appeals
Silence is interpreted as acceptance.
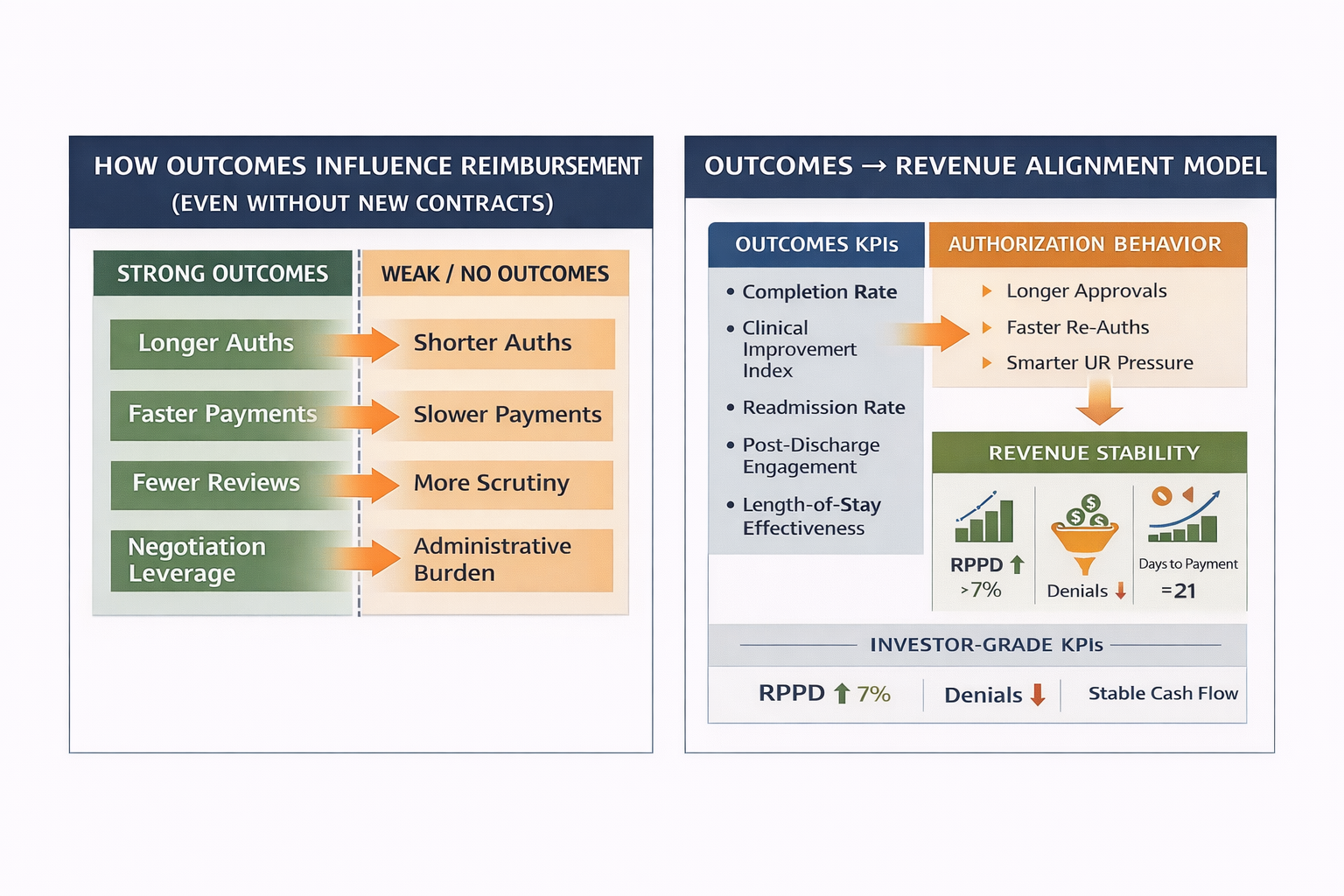
They Use Outcomes as Negotiation Leverage
Programs that can demonstrate:
- Clinical improvement
- Treatment completion
- Durable post-discharge outcomes
Experience:
- Fewer retro-denials
- More favorable reconsiderations
- Stronger standing in payer reviews
Outcomes data is no longer optional — it is currency.

The Hidden Risk: Compliance Without Leverage
Many organizations are fully compliant — yet financially exposed.
Why?
- Compliance ensures eligibility
- Leverage determines reimbursement quality
Leverage comes from:
- Data visibility
- Outcome measurement
- Payer-specific intelligence
Without leverage, programs absorb payer pressure silently.
Executive Warning Signs to Watch For
If leadership notices any of the following, payer behavior is already shifting:
- Stable census but declining net collections
- AR growing despite clean claims
- Fewer denials but more “adjustments”
- Increasing effort for the same reimbursement
These are not billing issues.They are payer strategy signals.
Final Executive Perspective
Payers rarely announce strategy changes.They test them.
Behavioral health organizations that wait for formal policy updates are already behind.
The future belongs to programs that:
- Track payer behavior as aggressively as revenue
- Measure outcomes alongside utilization
- Treat reimbursement as a strategic relationship — not a transaction
Seeing early is the advantage.
About Hartstone & Craft
Hartstone & Craft partners with behavioral health organizations to identify payer pressure early, protect reimbursement integrity, and build data-driven leverage in an increasingly constrained reimbursement environment.
We don’t wait for denials.We see the shift first.
.png)