Outcomes-Based Reimbursement in Behavioral Health
Why Proof of Effectiveness Is Becoming the New Currency
Executive Summary
Outcomes-based reimbursement is no longer a future concept in behavioral health — it is already shaping payer behavior, authorization decisions, and network participation.
While most programs still operate under fee-for-service assumptions, payers are quietly shifting toward performance-informed reimbursement, where clinical outcomes influence:
- Authorization length
- Payment velocity
- Rate negotiations
- Network inclusion
Programs that cannot demonstrate effectiveness will increasingly face tighter utilization controls and downward reimbursement pressure — even if they remain technically compliant.
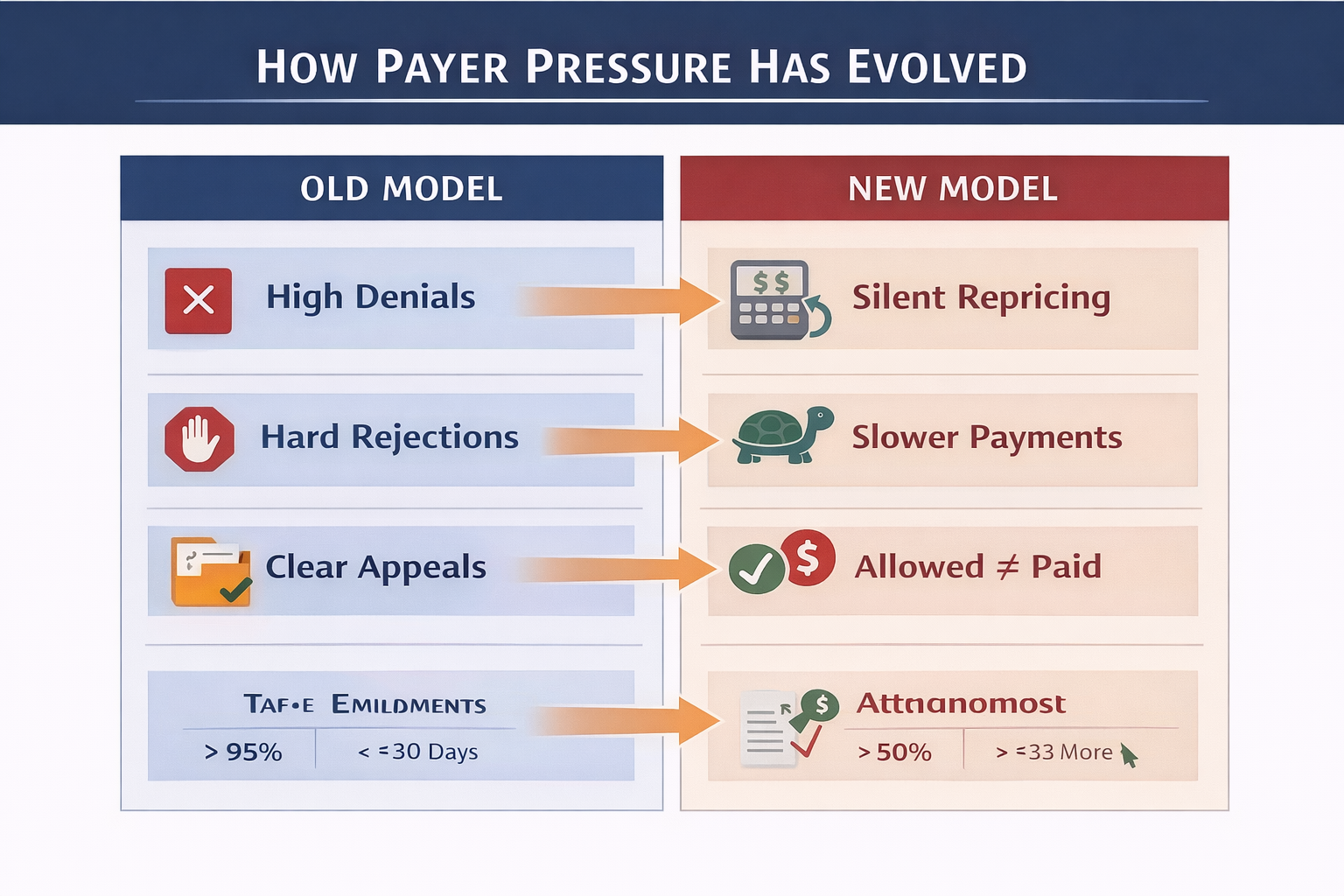
The Shift No One Announced
Unlike traditional reimbursement changes, outcomes-based models are not being rolled out through sweeping policy updates.
Instead, payers are:
- Benchmarking providers internally
- Comparing outcomes across networks
- Rewarding consistency quietly
- Applying pressure selectively
This allows payers to reduce cost without triggering widespread provider resistance.
Outcomes-based reimbursement is happening — just not where most programs are looking.
Why Behavioral Health Is a Primary Target
Behavioral health represents one of the fastest-growing cost centers in healthcare. At the same time, it has historically suffered from:
- Inconsistent outcome measurement
- Limited standardization
- Wide variance in length of stay
- High readmission risk
From a payer perspective, this creates both financial risk and opportunity.
Programs that can prove durable improvement become preferred partners. Those that cannot are quietly constrained.
What Outcomes-Based Reimbursement Really Means
Outcomes-based reimbursement does not necessarily mean pay-for-performance contracts — yet.
In practice, it looks like:
- Shorter initial authorizations for lower-performing programs
- Faster payment cycles for consistent performers
- Fewer retrospective reviews for trusted providers
- Increased scrutiny for programs with weak outcomes data
Outcomes are already influencing reimbursement behavior — even when contracts do not explicitly say so.
Core Outcome Metrics Payers Care About
1. Treatment Completion Rate
Measures the percentage of patients who complete a clinically appropriate course of care.
Why payers care:
- Strong proxy for engagement and effectiveness
- Correlates with reduced downstream utilization
Low completion rates often trigger tighter utilization controls.
2. Clinical Improvement (Pre- vs Post-Treatment)
Payers increasingly expect programs to track standardized clinical instruments, such as:
- PHQ-9
- GAD-7
- AUDIT / DAST
- ASAM reassessments
Key focus: Demonstrable, clinically meaningful change — not just service volume.
3. Readmission & Relapse Rates
Measured at 30, 60, and 90 days post-discharge.
Why it matters:
- High readmissions indicate ineffective or misaligned care
- Lower readmissions reduce payer cost over time
Programs that track and manage this metric gain credibility quickly.
4. Length-of-Stay Effectiveness
This compares clinical improvement achieved relative to days in treatment.
Why payers care:
- Identifies overutilization vs under-treatment
- Supports defensible authorization extensions
This metric directly affects utilization management decisions.
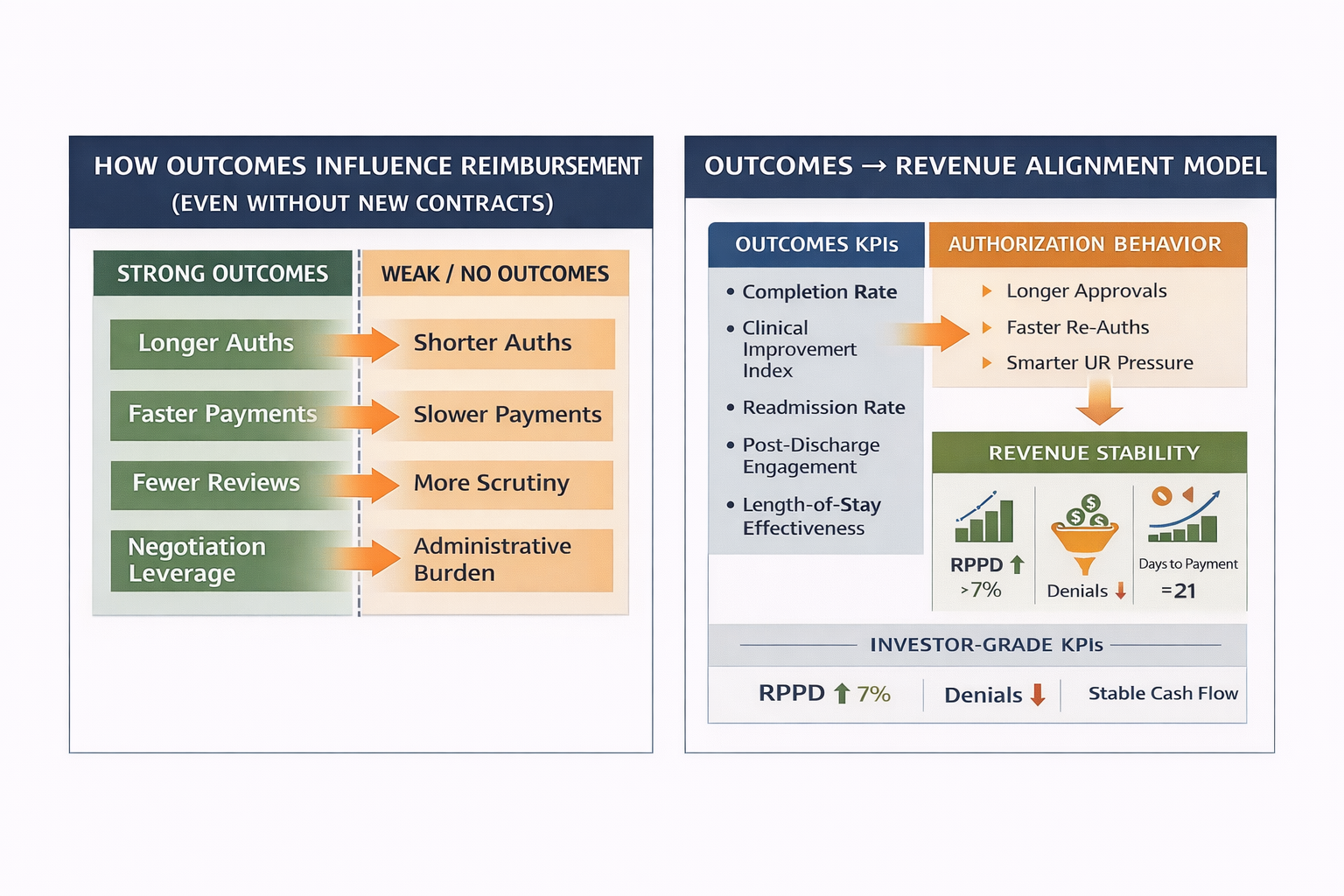
How Outcomes Influence Reimbursement (Even Without New Contracts)
Programs with strong outcomes typically experience:
- Longer authorization windows
- Faster claim adjudication
- Fewer retro-denials
- More constructive peer-to-peer reviews
Conversely, weak or absent outcomes data results in:
- Shortened authorizations
- Increased documentation demands
- Slower payments
- Higher administrative burden
This is reimbursement pressure by design.
The Most Common Mistake Programs Make
Many organizations treat outcomes as a clinical responsibility only.
High-performing programs treat outcomes as:
- An executive priority
- A payer negotiation asset
- A financial protection mechanism
Outcomes without leadership ownership lose strategic value.
Aligning Outcomes With Revenue & Operations
When outcomes KPIs are integrated with billing and utilization data, leadership gains:
- Stronger medical necessity narratives
- Data-backed appeal leverage
- Predictable authorization patterns
- Improved payer relationships
This alignment transforms outcomes from reporting requirements into strategic advantage.
What the Future Likely Holds
Over the next 3–5 years, behavioral health providers should expect:
- Increased outcomes benchmarking
- Network participation tied to performance
- Selective rate adjustments based on effectiveness
- Greater differentiation between providers
Programs that prepare now will lead. Those that wait will adapt under pressure.
Final Executive Perspective
Outcomes-based reimbursement is not about perfection — it is about proof.
Programs that can demonstrate meaningful, durable patient improvement will retain leverage in an increasingly constrained reimbursement environment.
Those that cannot will remain compliant — but vulnerable.
About Hartstone & Craft
Hartstone & Craft partners with behavioral health organizations to design outcome measurement frameworks that align clinical effectiveness with reimbursement strategy, payer relationships, and long-term sustainability.
Effectiveness is the future of leverage.
.png)