Behavioral health organizations operate in one of the most complex reimbursement environments in healthcare. Between commercial insurance, Medicaid, Medicare, Tricare, parity regulations, utilization management, and evolving payer rules, Revenue Cycle Management (RCM) has become a strategic discipline—not a back-office function.
This guide breaks down what effective behavioral health RCM actually looks like in 2026, where most organizations lose revenue, and how leadership teams can build systems that scale without sacrificing compliance or cash flow.
Understanding Behavioral Health Revenue Cycle Management
Behavioral Health Revenue Cycle Management refers to the end-to-end financial process that governs how a treatment program captures, bills, collects, and reports revenue.
This includes:
- Patient access and insurance verification
- Medical necessity and authorization management
- Accurate clinical documentation
- Coding and charge capture (CPT, HCPCS, Revenue Codes)
- Claims submission and follow-up
- Denial prevention and appeals
- Payment posting and reconciliation
- Patient financial responsibility workflows
- Financial reporting, KPIs, and forecasting
Unlike other healthcare verticals, behavioral health RCM must also align with ASAM levels of care, parity laws, and highly variable payer interpretations.
Why Behavioral Health RCM Fails in Most Organizations
Most revenue issues are not caused by low census or payer rates. They are caused by systemic breakdowns inside the revenue cycle.
The most common failure points we see include:
1. Weak Front-End Controls
- Incomplete benefit verification
- Missing exclusions or carve-outs
- Poor documentation of medical necessity
- Authorizations not aligned with actual services rendered
- Failing to gather Insurance Card and Imparitive patient information
Front-end errors compound downstream and often cannot be fixed after services are delivered.
2. Coding and Revenue Code Mismatches
Behavioral health billing is highly sensitive to:
- Incorrect revenue codes
- Mismatched CPT/HCPCS codes
- Incompatible Type of Bill (TOB) usage
- Incorrect place of service
Even small inconsistencies can trigger systematic denials or underpayments.
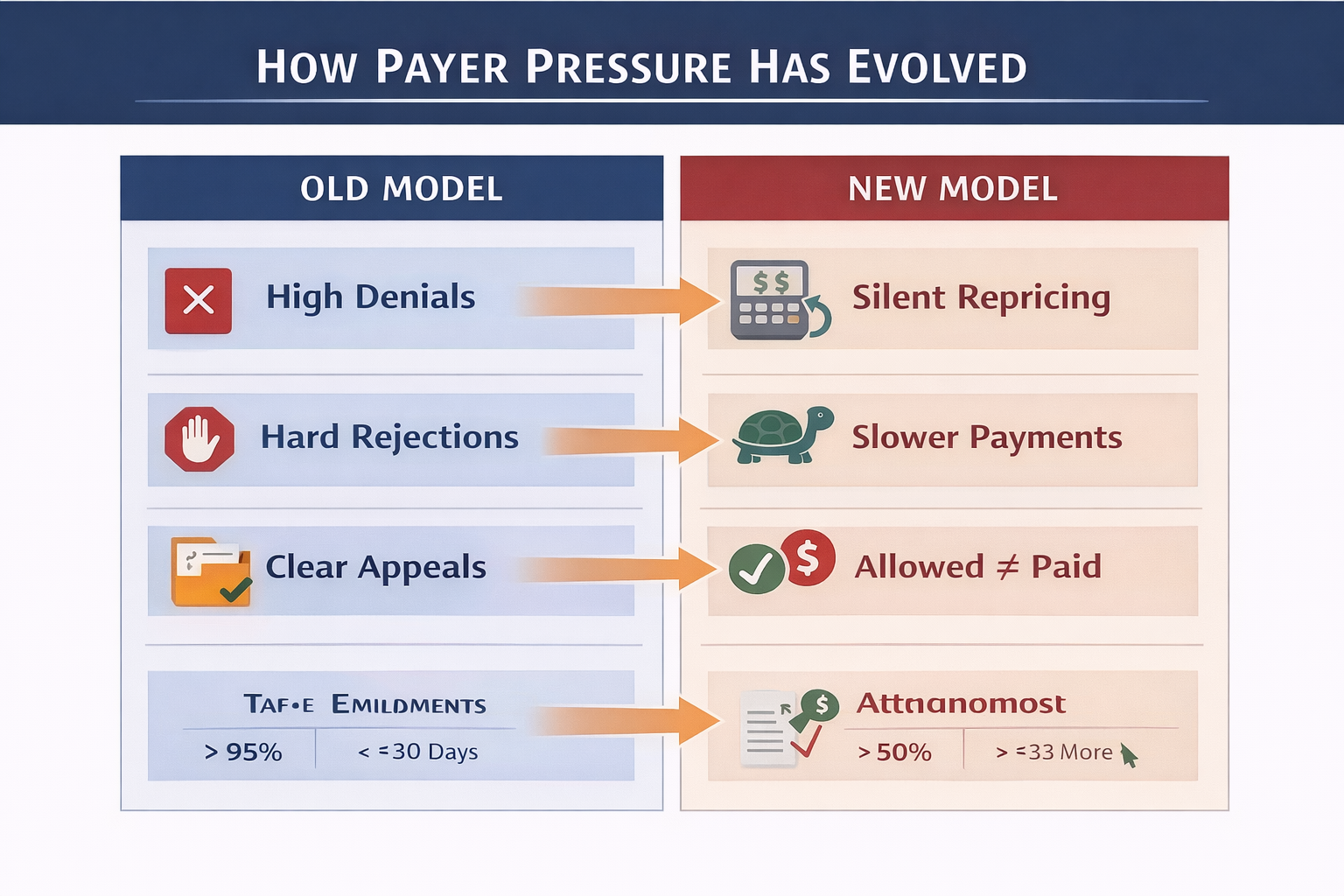
3. Denials Are Treated as “Normal”
Many organizations accept denial rates that would be unacceptable in other healthcare verticals. Denials are often:
- Tracked inconsistently
- Appealed without strategy
- Not analyzed by root cause
This creates predictable revenue leakage month after month.
4. No Executive-Level Visibility
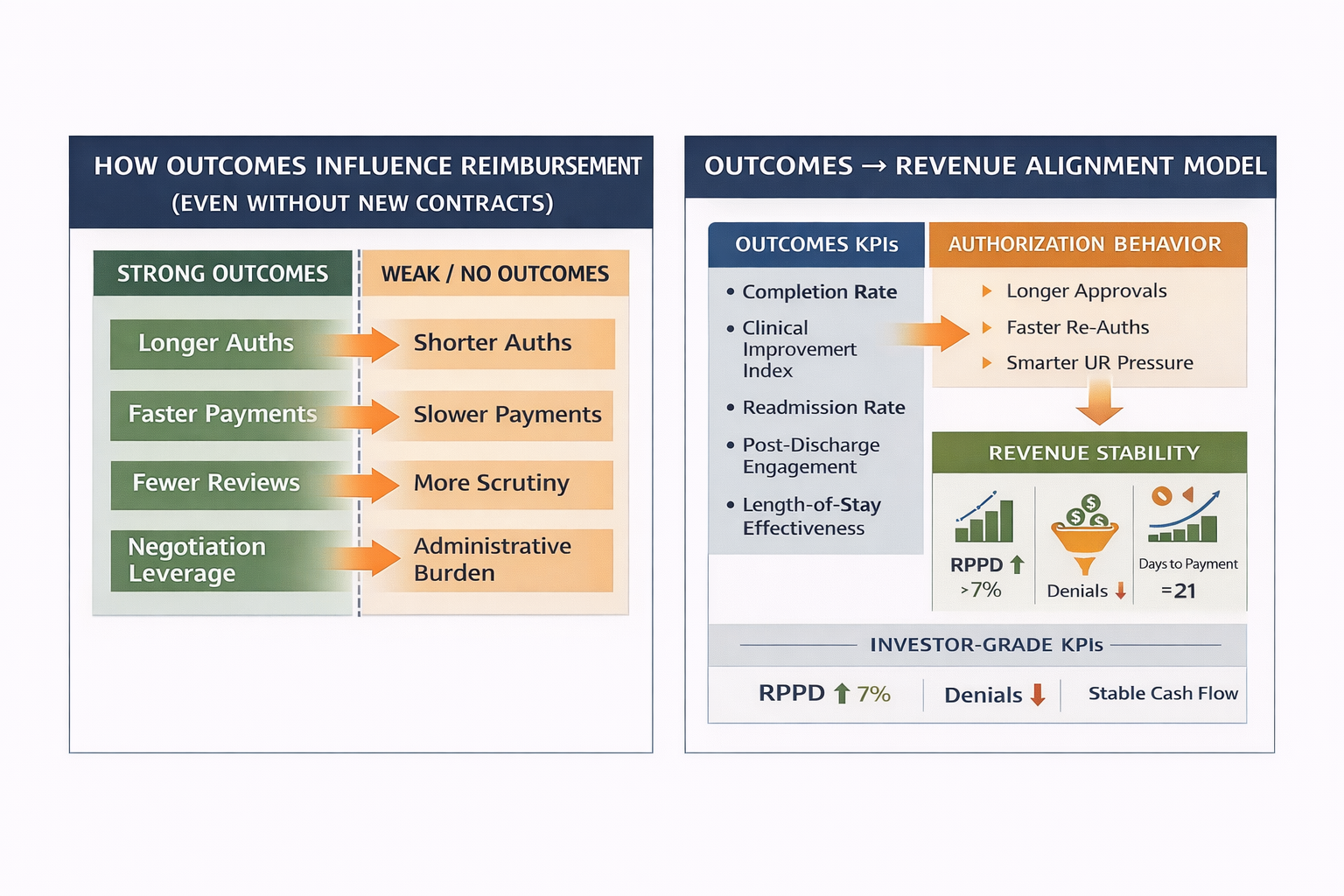
Leadership teams often rely on lagging indicators like bank balances or gross AR, instead of actionable KPIs such as:
- Clean claim rate
- Days to payment by payer
- Authorization utilization
- Underpayment variance
- Net revenue per patient day
Without visibility, decisions are reactive instead of strategic.
The Difference Between Outsourced RCM and High-Performance RCM
Outsourcing billing does not automatically solve revenue problems.
High-performance RCM—whether internal or outsourced—requires:
- Clearly defined workflows
- Payer-specific billing logic
- Documentation standards tied to reimbursement rules
- Real-time financial reporting
- Accountability across departments
Organizations that scale successfully treat RCM as revenue architecture, not clerical processing.
Core KPIs Every Behavioral Health Executive Should Track
At minimum, leadership should review:
- Clean Claim Rate (%)
- Average Days to Payment (by payer)
- Authorization Utilization Rate
- Denial Rate by Category
- Net Revenue per Patient Day
- Underpayment Recovery Rate
- Cash Collections vs. Expected Reimbursement
If these metrics are unavailable, unreliable, or delayed, the revenue system is already broken.
Compliance Is Not Optional—and It’s Not Static
Behavioral health RCM must operate within:
- Federal and state parity regulations
- Program licensing requirements
- Medical necessity standards
- Documentation integrity expectations
- Patient financial responsibility laws
Compliance failures often surface as financial problems first, long before audits or legal action occur.
How High-Growth Behavioral Health Organizations Structure RCM
High-performing organizations share several traits:
- RCM is integrated into clinical operations, not siloed
- KPIs are reviewed at the executive level, not just billing
- Documentation is designed for reimbursement, not just compliance
- Technology supports workflows, not the other way around
- Decision-makers understand payer behavior, not just rates
This alignment allows organizations to grow census, expand locations, and add payer contracts without collapsing cash flow.
Where Hartstone & Craft Fits In
Hartstone & Craft works with behavioral health organizations that need more than generic billing support.
Our work typically includes:
- RCM performance assessments
- KPI dashboard design
- Payer-specific revenue optimization
- Denial prevention frameworks
- Compliance-aligned documentation strategy
- Executive-level financial visibility
We operate at the intersection of strategy, operations, and revenue, helping leadership teams regain control of their financial systems.
Final Thought
Behavioral Health Revenue Cycle Management is no longer a back-office function. It is a core strategic capability that directly impacts growth, stability, valuation, and mission delivery.
Organizations that treat RCM seriously outperform those that don’t—consistently and predictably.
If your revenue feels unpredictable, opaque, or fragile, the system—not the market—is the problem.
Behavioral health organizations operate in one of the most complex reimbursement environments in healthcare. Between commercial insurance, Medicaid, Medicare, Tricare, parity regulations, utilization management, and evolving payer rules, Revenue Cycle Management (RCM) has become a strategic discipline—not a back-office function.
.png)