Why a 30‑Minute Medical Office Visit Can Be Paid $500+ — While a Full Day of Residential Treatment Struggles to Break $500
The Structural Reimbursement Imbalance No One in Behavioral Health Can Ignore
Executive Summary
In today’s healthcare reimbursement environment, it is not uncommon for a 20–30 minute outpatient medical visit to be reimbursed at $500 or more, while a 24‑hour day of residential behavioral health treatment — including housing, meals, clinical staffing, therapy, and supervision — struggles to secure contracted or allowable rates above the same amount.
This discrepancy is not accidental, and it is not based on clinical value alone.
It is the result of structural reimbursement design choices that systematically disadvantage behavioral health providers — particularly residential and higher levels of care.
Understanding why this imbalance exists is the first step toward correcting it.

The Question Behavioral Health Leaders Are Asking
How can a brief office visit command higher reimbursement than an entire day of intensive, round‑the‑clock treatment?
From a care‑delivery perspective, the disparity defies logic.
From a reimbursement perspective, it makes perfect sense — once the system is understood.
How a 30‑Minute Medical Visit Reaches $500+
1. RVU‑Driven Valuation Favors Physician Time Over Systemic Care
Most outpatient medical visits are reimbursed using Relative Value Units (RVUs), which reward:
- Physician time
- Decision complexity
- Perceived liability
- Historical specialty influence
Evaluation & Management (E/M) codes are heavily weighted toward individual physician activity, not total cost of care.
As RVU values increase, reimbursement follows — even when the visit duration is short.
2. Medical Services Are Anchored to Medicare Benchmarks
Commercial payers frequently price medical services at multiples of Medicare rates.
Because Medicare:
- Regularly updates physician fee schedules
- Actively protects access to medical specialties
- Responds quickly to provider lobbying
Medical visit reimbursement continues to rise.
Behavioral health, by contrast, has historically lagged behind in federal rate modernization.
3. Simplicity of Billing Drives Payment Certainty
A medical office visit typically involves:
- One provider
- One CPT code
- One encounter
This simplicity reduces payer friction, audit risk, and administrative burden — all factors payers reward with faster, higher reimbursement.
Why Residential Behavioral Health Is Paid So Poorly
1. Residential Care Is Treated as a Cost Center, Not a Clinical Asset
From a payer perspective, residential treatment is viewed as:
- High‑cost
- Long‑duration
- Difficult to standardize
Rather than valuing outcomes or intensity, payers focus on cost containment.
This leads to:
- Aggressive per‑diem caps
- Repricing to “reasonable” benchmarks
- Resistance to market‑rate contracts
2. Per‑Diem Rates Flatten Clinical Complexity
Residential reimbursement is often paid on a per‑diem basis, which:
- Ignores daily variation in clinical intensity
- Bundles multiple services into a single rate
- Removes incentives for individualized care
A patient receiving multiple therapy hours, medical oversight, and crisis intervention may be reimbursed the same as a clinically stable patient — by design.
3. Behavioral Health Lacks Pricing Power
Medical specialties have spent decades:
- Building strong advocacy organizations
- Influencing CMS valuation
- Establishing clear specialty‑specific benchmarks
Behavioral health has not enjoyed the same leverage.
The result is a reimbursement structure that undervalues comprehensive treatment while overvaluing discrete medical encounters.
The Role of Payer Strategy in Widening the Gap
Payers have learned that:
- Residential providers are capacity‑constrained
- Patients lack alternatives at higher levels of care
- Providers will often accept lower rates to maintain census
This shifts negotiating power decisively toward payers.
When residential programs push back, payers increasingly respond with:
- Silent repricing
- Shortened authorizations
- Delayed payments
The imbalance deepens.
Why This Is a Problem Beyond Fairness
This reimbursement gap does more than frustrate providers.
It:
- Discourages investment in residential treatment
- Drives staff burnout and turnover
- Forces programs to operate on unsustainable margins
- Undermines treatment quality over time
In effect, the system rewards brief medical interactions more than sustained recovery work.
The Path Forward: What Must Change
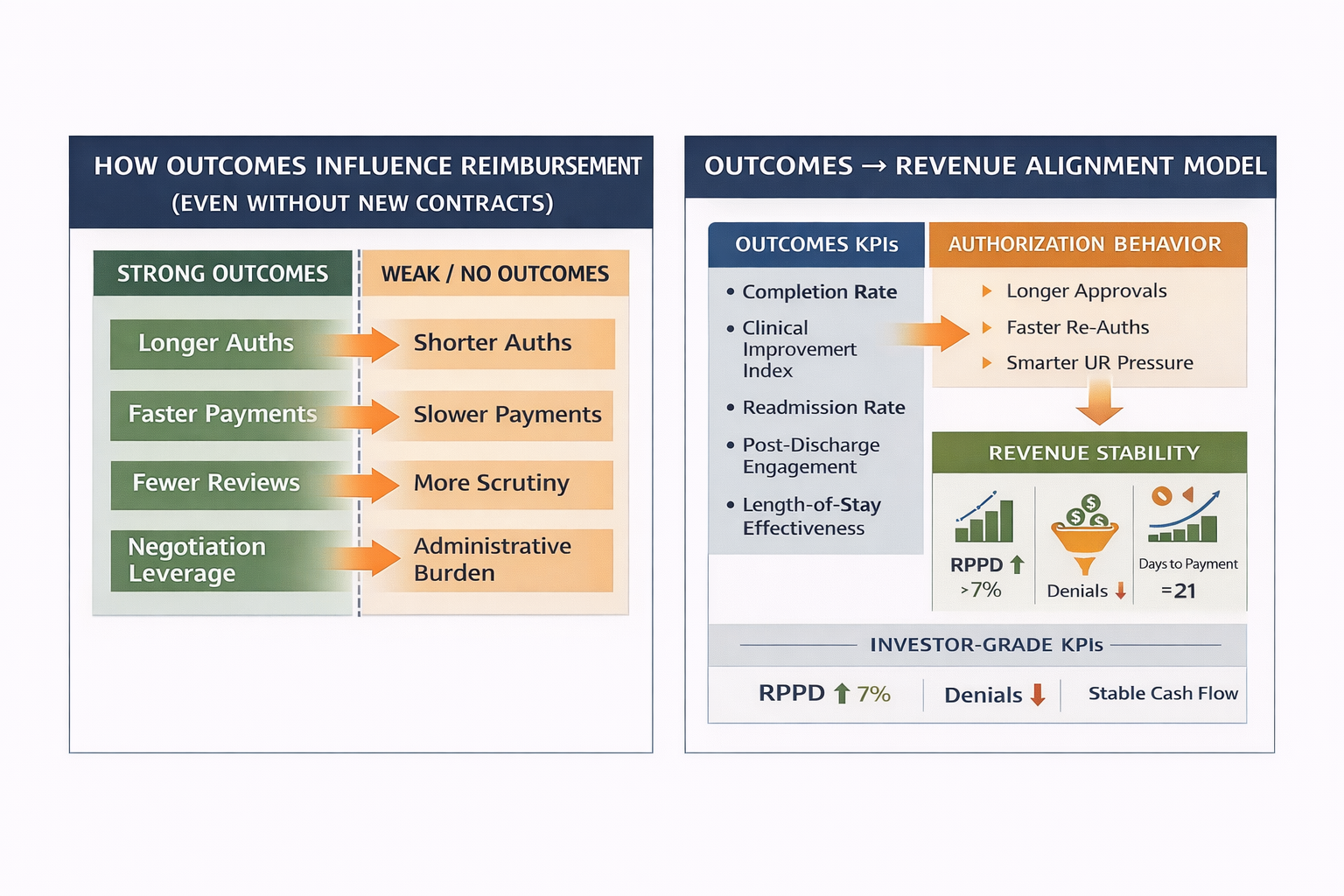
1. Residential Care Must Be Reframed as Outcome‑Critical
Programs that can demonstrate:
- Reduced readmissions
- Durable recovery outcomes
- Lower downstream medical utilization
Gain leverage in negotiations.
Outcomes are the strongest counterweight to per‑diem suppression.
2. Data Must Replace Appeals
Residential providers must move beyond reactive appeals and toward:
- Market‑rate benchmarking
- Outcome‑adjusted value narratives
- Payer‑specific performance data
Negotiation must be evidence‑driven.
3. Pricing Power Must Be Rebuilt
This requires:
- Collective data intelligence
- Executive‑level payer strategy
- Refusal to normalize unsustainable rates
Without pricing power, reimbursement will continue to drift downward — regardless of care quality.
Final Executive Perspective
The fact that a 30‑minute medical visit can command higher reimbursement than a full day of residential behavioral health treatment is not a reflection of value.
It is a reflection of how the system was built — and who it was built for.
Until residential behavioral health is positioned as a clinical necessity with measurable economic impact, the imbalance will persist.
Programs that understand this reality — and respond strategically — will survive.
Those that don’t will remain trapped between rising costs and suppressed reimbursement.
About Hartstone & Craft
Hartstone & Craft partners with behavioral health organizations to analyze reimbursement inequities, strengthen payer negotiations, and reposition residential care as an outcome‑driven, economically defensible component of the healthcare continuum.
Fair reimbursement is not a demand.
It is a strategy.
.png)