Underpayments Are Now a Bigger Risk Than Denials in Behavioral Health
Why Revenue Is Leaking Even When Claims Are “Paid”
Executive Summary
For years, behavioral health organizations were trained to fear denials.
Denied claims were visible, disruptive, and painful — but they were also obvious. Today, the most dangerous revenue threat is quieter, harder to detect, and far more expensive:
Underpayments.
Many programs now experience lower denial rates than ever before, yet net collections continue to decline. This is not coincidence. It is the result of a structural shift in payer strategy.
Underpayments now represent a larger and more consistent source of revenue loss than denials — and most organizations are not tracking them.
The Old Model: Denials as the Primary Threat
Historically, revenue cycle risk in behavioral health looked like this:
- Claims denied for authorization or medical necessity
- Appeals submitted
- Revenue recovered (or written off)
Denials were disruptive, but they were detectable.
Leadership could see the problem, allocate resources, and measure recovery.
The New Model: Claims Are Paid — Just Not Correctly
Today, many behavioral health programs report:
- Stable or improving denial rates
- High clean-claim percentages
- Fewer outright rejections
Yet collections are falling.
Why?
Because claims are increasingly being:
- Repriced after adjudication
- Paid below contracted or historical rates
- Adjusted without clear explanation
The claim is “paid,” so alarms never trigger.
Why Payers Prefer Underpayments to Denials
Underpayments are strategically superior from a payer perspective.
They:
- Reduce provider backlash
- Lower appeal volume
- Normalize reduced reimbursement quietly
- Shift the burden of detection to providers
Most providers never challenge them.
Silence is interpreted as acceptance.
The Financial Impact Most Programs Miss
Denials tend to be episodic.
Underpayments are systemic.
Across mid-sized behavioral health programs, we routinely observe:
- 3–8% leakage on allowed amounts
- Hundreds of thousands in unrecovered revenue annually
- Gradual margin erosion that leadership cannot explain
Because underpayments don’t disrupt workflows, they persist indefinitely.
Common Sources of Underpayments in Behavioral Health
1. Repricing Algorithms & Third-Party Vendors
Repricing entities apply payer-defined “reasonable” benchmarks that often:
- Ignore market rates
- Discount behavioral health disproportionately
- Vary widely by payer and episode length
Without negotiation, these become de facto rate cuts.
2. Contract Misalignment & Silent Adjustments
Even in-network providers experience:
- Misapplied fee schedules
- Incorrect per-diem calculations
- Partial payments across multi-day episodes
Most organizations do not audit contract compliance at scale.
3. Bundled vs Unbundled Service Variance
Behavioral health billing often involves complex combinations of:
- Per-diem rates
- Hourly group services
- Ancillary clinical components
Small discrepancies compound quickly.

Why Most Organizations Don’t Catch Underpayments
Underpayments persist because:
- AR teams focus on denials, not variance
- Allowed vs paid is rarely audited
- Reporting systems don’t flag subtle discrepancies
- Finance assumes payment accuracy
In many organizations, no one owns underpayment detection.
What High-Performing Programs Do Differently
They Treat Underpayments as Strategic Risk
Sophisticated organizations:
- Track allowed vs paid by payer
- Audit underpayments monthly
- Escalate trends early
- Negotiate repriced claims aggressively
They do not assume accuracy.
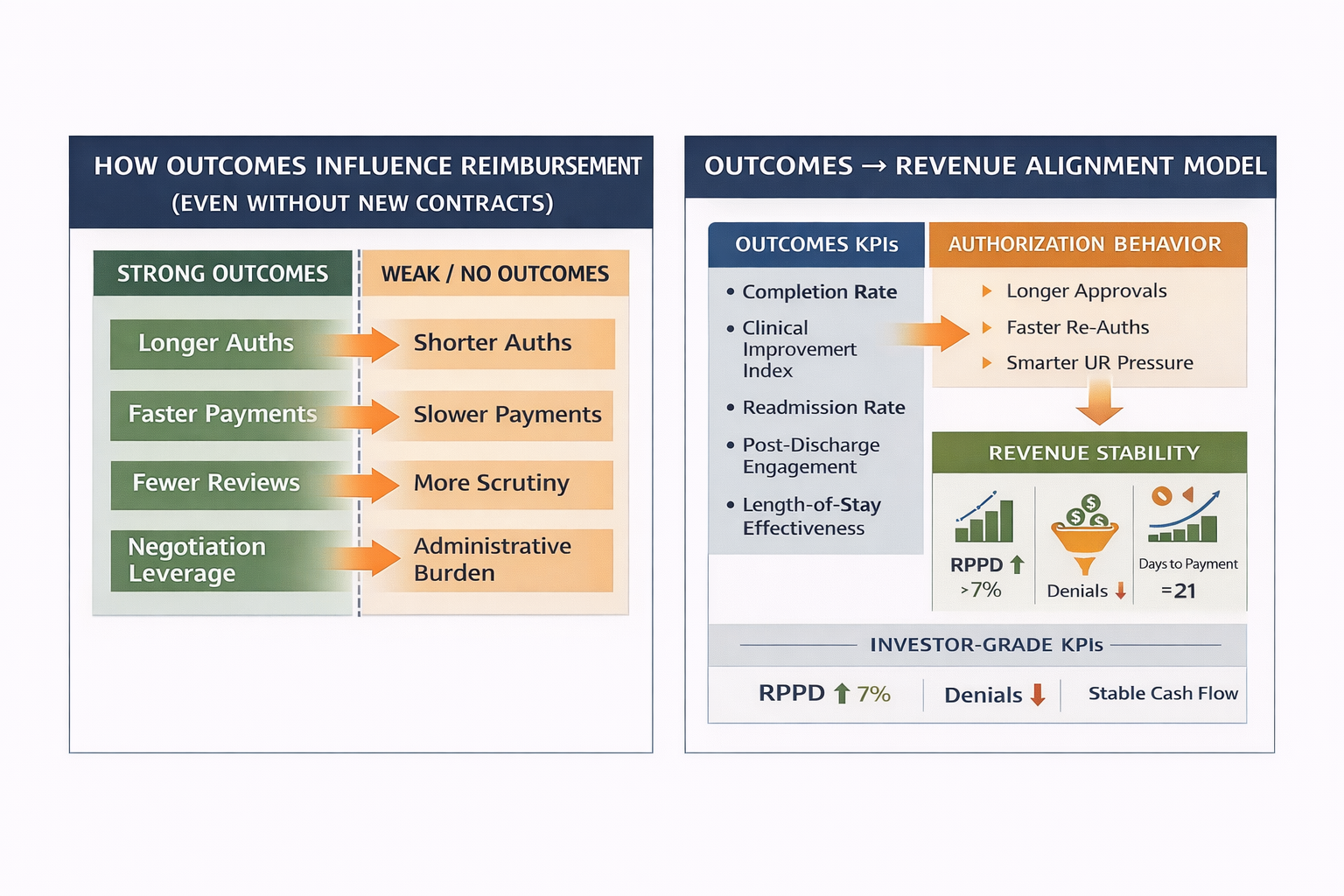
They Use Data as Leverage
Programs with strong documentation, outcomes data, and utilization discipline:
- Recover higher percentages in reconsideration
- Face less resistance in negotiations
- Build payer credibility over time
Data changes the conversation.
Executive Warning Signs
If leadership sees any of the following, underpayments are likely occurring:
- Declining net collection rate without denial spikes
- AR balances growing despite clean claims
- Revenue per patient day trending down
- More “adjustments” than denials on EOBs
These are not billing failures.
They are pricing failures.
Final Executive Perspective
Denials are loud.
Underpayments are quiet.
But underpayments are far more dangerous.
Organizations that fail to detect and challenge them experience gradual, irreversible margin erosion — even while believing their revenue cycle is healthy.
The future belongs to programs that:
- Measure payment accuracy
- Challenge silent repricing
- Treat reimbursement as a strategic negotiation
Anything less is passive acceptance.
About Hartstone & Craft
Hartstone & Craft partners with behavioral health
.png)